What is the excluded provider list and who is on it?
The excluded provider list is a list of individuals or entities that are not eligible to participate in federal healthcare programs due to conduct that violates laws, regulations, or policies. The individuals or entities on the list are excluded from receiving payment from Medicare, Medicaid, or other federal health programs for the provision of healthcare services. The list is maintained by the Office of Inspector General (OIG) of the Department of Health and Human Services (HHS) and includes providers who have been excluded due to criminal convictions, fraudulent billing practices, patient abuse or neglect, and other prohibited activities.
Why does our organization need to do this?
Compliance with regulations
Healthcare organizations must follow strict regulations set by government agencies such as the Office of Inspector General (OIG) and the Department of Health and Human Services (HHS). Exclusion list checking helps organizations verify that they are not employing individuals who are excluded from participating in federally funded healthcare programs.
Patient safety
Exclusion list checking helps prevent patients from receiving care from individuals who have been excluded from participating in healthcare programs due to disciplinary actions, such as license revocation or criminal convictions.
Protecting organization's reputation
Healthcare organizations that employ excluded individuals can face significant penalties and fines, and can also harm their reputation. Exclusion list checking helps organizations avoid these consequences by ensuring that they are employing only eligible individuals.
Ethical considerations
Exclusion list checking is also important from an ethical perspective, as healthcare organizations have a responsibility to provide quality care to patients and to avoid employing individuals who have a history of unethical behavior.
What happens if my organization fails to check our business involved entities?
If a business fails to check the excluded provider list before employing or contracting with a healthcare provider, they may be at risk of violating federal law and facing serious consequences. These can include:
Civil Monetary Penalties
The OIG can impose penalties for knowingly employing or contracting with excluded individuals or entities.
Repaying Medicare/Medicaid Overpayments
The business may be required to repay any Medicare or Medicaid payments received for services provided by an excluded provider.
Exclusion from Federal Health Programs
The business itself may be excluded from participating in federal health programs if it is found to have knowingly employed or contracted with an excluded provider.
False Claims Act Liability
The business may be liable under the False Claims Act for submitting claims for services provided by an excluded provider.
Checking the excluded provider list is a requirement under federal law and is considered a best practice in the healthcare industry to help ensure that individuals and entities with a history of fraud or other prohibited activities do not participate in federal health programs.
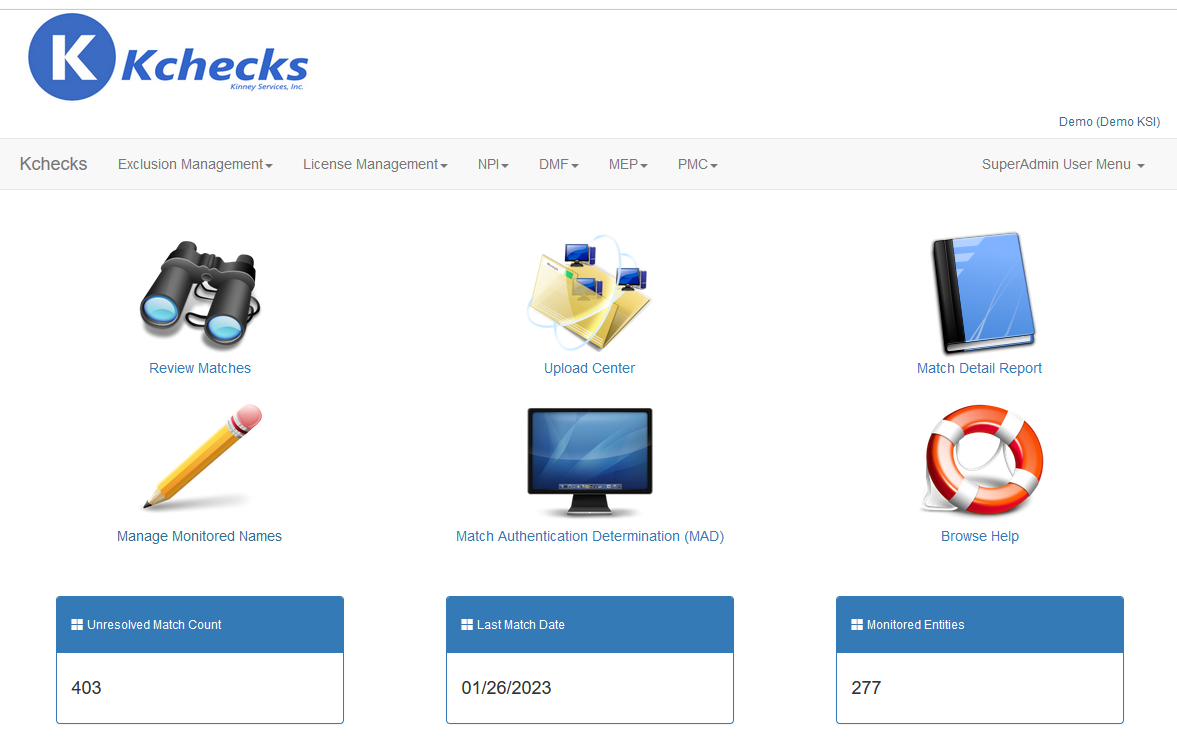
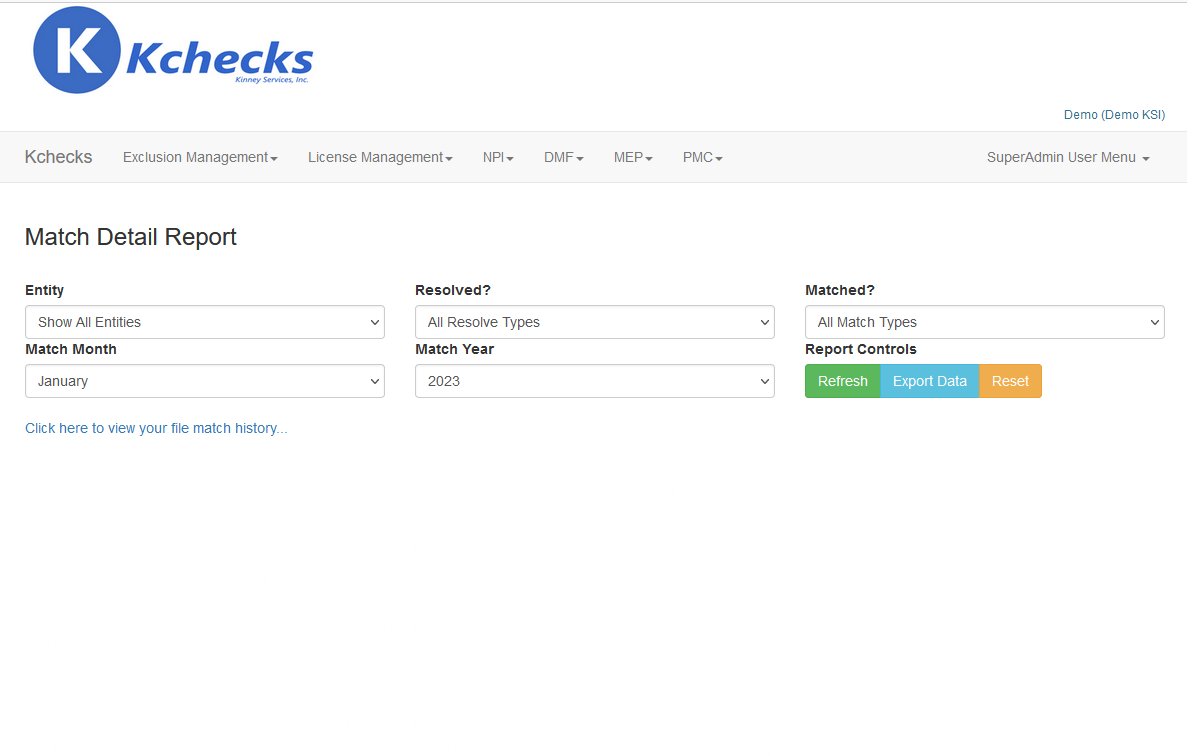
Kchecks to the rescue
We handle all of the difficult matching and reporting so you don't have to.
Let our years of experience benefit you and your company.
To learn more, you can reach a sales representative by using our contact form or by phone at +1 (518) 371-0176